Cancer Patients
Patients with cancer have a sixfold increased risk of VTE compared to those without cancer. Active cancer accounts for almost 20% of all new VTE events occurring in the community. Furthermore, VTE is one of the most common complications seen in cancer patients. Unfortunately, there are few data that allow one to predict which cancer patients will develop VTE. The risk varies by cancer type, and is especially high among patients with malignant brain tumors and adenocarcinoma of the ovary, pancreas, colon, stomach, lung, prostate, and kidney. However, more specific risk estimates of VTE by cancer type, stage, and treatment approaches are still largely unknown. 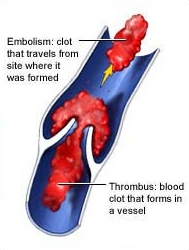
As discussed in other sections of this article, cancer patients undergoing surgery have at least twice the risk of postoperative DVT and more than three times the risk of fatal PE than noncancer patients who are undergoing similar procedures viagra and cialis online. Cancer is also an independent predictor of lack of response to prophylaxis (ie, the development of postoperative DVT despite the use of prophylaxis).
There is strong evidence that LDUH effectively reduces the risk of DVT and fatal PE following cancer surgery. LMWH is at least as efficacious as LDUH in surgical oncology patients. In cancer surgery, the dose of prophylactic anticoagulants is important. For example, among gynecologic oncology patients, dosing of LDUH three times daily was more efficacious than twice-daily dosing. Among general surgical patients with underlying malignancy, prophylaxis with dalteparin, 5,000 U SC once daily, was more efficacious than with a dose of 2,500 U. Two clinical trials in cancer surgery patients have shown that the continuation of LMWH prophylaxis for 3 weeks after hospital discharge reduced the risk of late venographic DVT by 60%.
Nonsurgical cancer therapies also increase the risk of VTE. For example, in two large clinical trials of women with node-negative breast cancer, the 5-year incidence of VTE was 0.2% in those who received placebo, 0.9% in those who received tamoxifen, and 4.2% in those who received tamoxifen plus chemotherapy. Furthermore, the risk of VTE in women with stage II breast cancer declined dramatically once chemotherapy was complet-ed. Compared to patients without cancer, those receiving cytotoxic or immunosuppressive therapy have a 6.5-fold increased risk of VTE. Cancer patients receiving chemotherapy account for 13% of the overall burden of VTE in the population. In the only clinical trial of thromboprophylaxis during chemotherapy, 311 women with metastatic breast cancer received either very-low-dose warfarin (INR range, 1.3 to 1.9) or placebo.